The world’s first gene therapy has been approved by the UK’s drugs authority as a possible treatment for two inherited blood illnesses.
The first gene-editing technology to be licenced, Casgevy, treats sickle cell disease and beta thalassemia. Its developers, Crispr, were awarded the 2020 Nobel Prize for this tool.
The medication is for patients 12 years of age and older, according to the Medicines and Healthcare Products Regulatory Agency (MHRA), “after a rigorous assessment of its safety, quality and effectiveness.”
What is sickle cell disease and beta thalassemia?
The hereditary disorders sickle cell disease and beta thalassemia are brought on by defects in the haemoglobin gene, which is responsible for red blood cells’ ability to transport oxygen throughout the body.

While beta thalassemia mostly affects persons of Mediterranean, south Asian, south-east Asian, and Middle Eastern descent, sickle cell disease is more frequent in those with an African or Caribbean familial history.
Sickle cell disease can cause anaemia, severe and sometimes fatal infections, and excruciating pain.
Severe anaemia can occur in people with beta thalassemia. In addition to receiving regular injections and medications, patients frequently require a blood transfusion every three to five weeks.
How does the gene tool work?
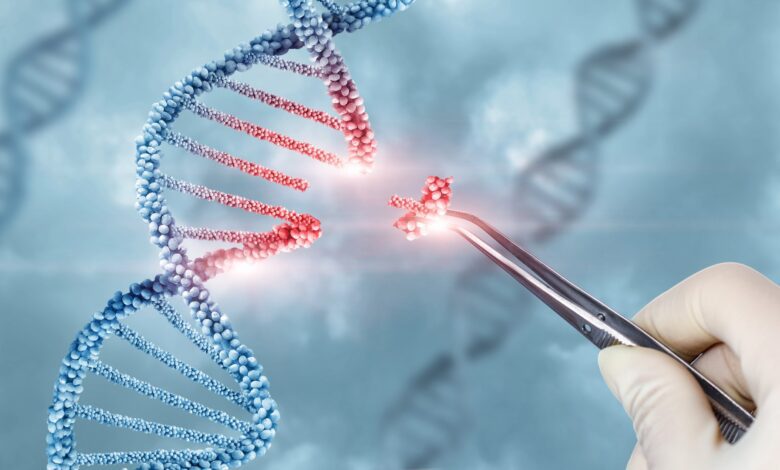
Casgevy’s mechanism of action involves correcting the defective gene in a patient’s bone marrow stem cells, enabling the body to create healthy haemoglobin. This DNA can be precisely manipulated by scientists thanks to gene editing.
In order to employ Casgevy, medical professionals remove blood-forming stem cells from patients’ bone marrow. The genes that provide the instructions for producing haemoglobin in those cells are then edited using a type of molecular scissors called CRISPR-Cas9. The precise cuts made by this editing tool are guided to the correct location in the DNA by an RNA molecule.
To put it simply, Cas9 breaks both sides of the DNA when it reaches the BCL11A gene, which is the target of Casgevy. Usually, BCL11A prevents the production of a certain form of haemoglobin that is exclusively produced in foetuses.
Casgevy alters this gene to enable the production of foetal haemoglobin, which differs from adult haemoglobin and is free of the same flaws found in beta thalassaemia and sickle-cell disease patients.
Up until now, the only choice for permanent therapy has been a bone marrow transplant, which requires a donor who is precisely matched and entails a risk of rejection. In order for this to function, bone marrow stem cells are extracted, altered in a laboratory, and subsequently reinfused into the patient, potentially curing them.
According to the MHRA, most patients’ healthy haemoglobin production was restored with cassenvy in clinical studies.
After receiving medication for at least a year, 28 out of 29 participants (97%) in the sickle cell disease clinical study reported being pain-free.
Ninety-three percent (39 out of 42 patients) in the beta thalassemia clinical study did not require a red blood cell transfusion for at least a year following their therapy. In the remaining three, red cell transfusion requirements were lowered by more than 70%.
“There are limited medicines currently available to patients, so I welcome today’s news that a new treatment has been judged safe and effective, which has the potential to significantly improve the quality of life for so many.” John James, the Sickle Cell Society’s main executive.
Both disorders “are painful, life-long conditions that in some cases can be fatal,” according to Julian Beach, interim executive director of healthcare quality and access at the MHRA.
“To date, a bone marrow transplant – which must come from a closely matched donor and carries a risk of rejection – has been the only permanent treatment option,” he continued.
““Sickle cell disorder is an incredibly debilitating condition, causing significant pain for the people who live with it and potentially leading to early mortality. There are limited medicines currently available to patients, so I welcome today’s news that a new treatment has been judged safe and effective, which has the potential to significantly improve the quality of life for so many,” stated John James, chief executive of the Sickle Cell Society.
The therapy has not yet been investigated for broader NHS usage.
“Today is a historic day in science and medicine: this authorisation of Casgevy in Great Britain is the first regulatory authorisation of a Crispr-based therapy in the world,” said Reshma Kewalramani, president of Vertex, which co-launched the medication with Crispr Therapeutics.
“We’re delighted this world-first therapy has been granted an MHRA licence, which brings us a step closer to it being available to people with severe sickle cell disease in the UK. Patients won’t be able to access Casgevy on the NHS until it is approved by Nice. We hope that Nice will listen to patients with severe sickle cell disease who desperately need better treatment options and make this innovative therapy available as quickly as possible.”” said Yasmin Sheikh, head of strategy and public relations at Anthony Nolan.
You might also be intersted in – What is Disease X, and could it be 20 times deadlier than Covid-19?